We’ve all felt a little queasy after taking too many helpings of our favorite food. But if you’re always feeling nauseous after eating, there may be something else going on. Experts share 10 reasons why you may be feeling uneasy after chowing down.
Eating shouldn’t be a painful experience. Of course, we all feel a little bloated now and then after a meal, and that’s usually normal—maybe you overindulged a bit at a restaurant because that flourless chocolate cake looked too good to pass up, or you unintentionally ramped up your fiber intake when you went for a second serving of three-bean chili. In these cases, the pain is relatively fleeting and has a clear cause.
But always feeling nauseous after eating (think: bloating, gas, nausea) could be a red flag for an underlying condition or that you need to adjust your habits. Even if you think you’re eating well, a variety of factors—from what you eat to when you eat to how you eat—could be setting you up for post-meal pain.
Here, we talked to gut health experts about potential reasons you’re feeling nauseous after eating and what you can do about them.
10 Reasons You’re Feeling Nauseous After Eating

If your stomach hurts after eating, there are a few reasons it may be happening. Whether you’re experiencing bloating after eating or you feel like throwing up after eating, here are 10 potential causes.
1. You’re Not Chewing Enough.
Given all of our modern distractions, it’s no wonder we scarf down food in two or three bites. (When was the last time you actually ate lunch without scrolling Instagram or checking your email?) But swallowing your food without adequately chewing can overwhelm your stomach, potentially priming you for gas, bloating, and nausea. “If you don’t chew enough, the entire digestive process is slowed down, impaired, and likely ineffective,” says Nikki Yelton RD, LDN, CNHP, a functional medicine dietitian with a focus on gut health.
That’s because chewing is a crucial first step in the digestive process. “When you chew thoroughly, your food is exposed to saliva for longer periods of time and the [digestive] enzymes in your saliva help break down your food before you even swallow,” explains Yelton. Chewing more will put less strain on the rest of the digestive process and may even help you absorb more nutrients from the foods you eat.
Try this: Aim to chew each bite of food at least 15-25 times, suggests Yelton. “When chewing is a priority, you’ll likely notice many health benefits such as fewer feelings of bloat and indigestion after meals, regulated appetite, true feelings of fullness, and a healthier gut microbiome due to epithelial growth factor (EGF) production,” she says. (EGF is a protein released in saliva that stimulates the growth and repair of epithelial tissue, including the intestinal epithelium.)
2. You’re Stressed Out or Anxious.

Constantly asking yourself “Why do I feel nauseous after eating?” Your stress levels might be to blame. Unmanaged stress can trigger a cascade of processes that wreak havoc on the digestive system and make you feel ill after a meal.
Your gut and brain actually communicate back and forth via the gut-brain axis. So when you’re stressed and your body enters fight-or-flight mode (releasing hormones like cortisol and norepinephrine that are meant to prepare you for action), your digestion is impacted as well.
Often, this leads to changes in gastrointestinal motility, or how quickly food moves through the GI tract, which can lead to either constipation or diarrhea, according to Marvin Singh, MD, an integrative gastroenterologist and precision medicine expert. “Chronic stress can also impact the composition of the gut microbiome,” he says. “There’s been research to suggest when you have these stress chemicals released in the gut, they can contribute to non-pathogenic bacteria becoming more pathogenic. So basically, bacteria that might not be causing you any trouble could now change and become more problematic to you as a result of all the stress.”
According to Yelton, chronic exposure to stress also “directly results in changes in the brain-gut interactions, which leads to the development of GI disorders including inflammatory bowel disease (IBD), irritable bowel syndrome (IBS), and intestinal permeability, or leaky gut.”
Try this: “Adopting effective stress management techniques is essential,” says Yelton. “Start by setting boundaries—learn your limits and when to say ‘no’.” Deep breathing (when you’re feeling stressed and right before meals), evening Epsom salt baths, and practicing yoga are also great ways to release tension in the body and refocus the mind, she says.
3. Your Gut Microbiome Is Out of Balance.
Your gut microbiome is home to trillions of bacteria and other microorganisms that influence your health in important ways. When the ratio of these microbes gets thrown out of whack or bacteria starts growing where it shouldn’t (as is the case with SIBO)—which can be due to everything from stress to poor food choices to medication to underlying health conditions—you can experience a range of problematic post-meal symptoms.
“You might experience nausea, bloating, gas, burping, abdominal distension, and constipation or diarrhea—or a little of both,” says Dr. Singh. A bacterial imbalance in your gut microbiome can also set you up for leaky gut—when the gut lining becomes damaged and loosens, allowing substances that should remain within the gut to leak into the bloodstream and setting you up for gut infections, food sensitivities, and nutrient deficiencies, explains Yelton.
Leaky gut, in turn, can drive inflammation that further contributes to an imbalanced gut, causing a vicious cycle. “This results in the digestive system being chronically unhappy, hence chronic bloating every time you eat,” says Yelton.
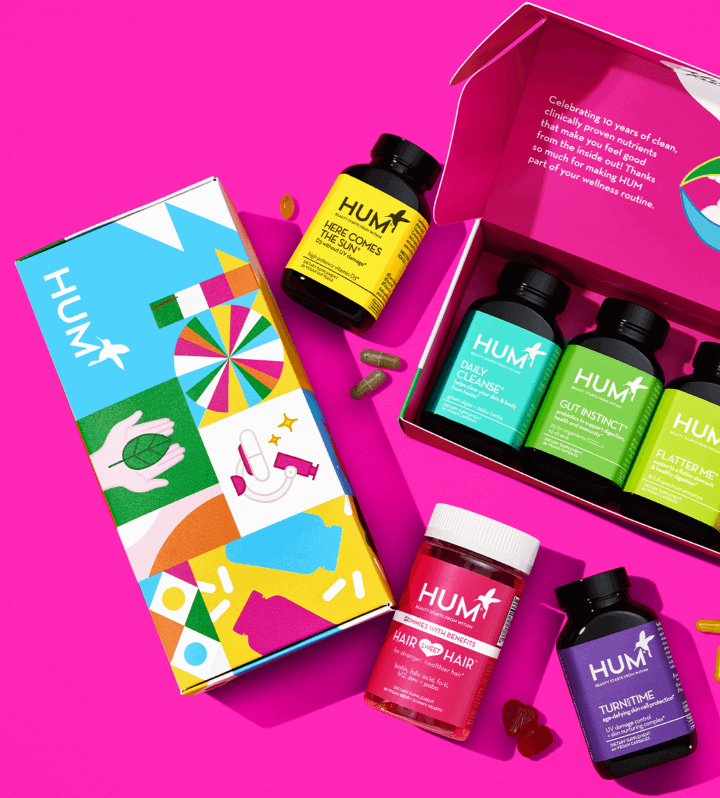
Try this: There’s no one way to heal or balance the gut. Both Yelton and Dr. Singh recommend seeking the help of an integrative or functional medicine practitioner who can identify your unique imbalances and potential underlying conditions, and come up with a custom healing protocol. Consuming a fiber-rich diet with a variety of plant foods, getting regular physical activity, and taking a probiotic supplement with several different strains of beneficial bacteria (like HUM’s Gut Instinct) are good preventive measures to help keep your gut in balance before you develop a problem.
4. You Have GERD or Acid Reflux.
If you’re experiencing a painful burning sensation in the middle of your chest that gets worse after eating, along with nausea, burping, and a sour taste in your mouth, it could be acid reflux (a.k.a. heartburn). “Acid reflux occurs when the contents of your stomach that have not been broken down by stomach acid are pushed back up into the esophagus, and the acidity of the contents then burns the esophageal lining,” says Yelton.
“Heartburn and acid reflux after eating are actually often triggered by low stomach acid rather than too much. When levels of stomach acid are too low, the stomach and digestive tract are unable to properly digest food.” Certain foods and beverages (including alcohol), as well as overeating, may also contribute to acid reflux, adds Dr. Singh.
And when acid reflux occurs repeatedly, it turns into GERD (gastroesophageal reflux disease, or chronic acid reflux). “After too many bouts of acid reflux, it damages your esophagus,” says Yelton. “This causes dysfunction of the lower esophageal valve that separates the esophagus and stomach. Once the valve becomes damaged, the food and acid [from your stomach] are able to make their way up to your esophagus on a chronic basis.”
Try this: Try diluting one to two teaspoons of apple cider vinegar (ACV) with water and drink it before your meals, suggests Yelton. Acid reflux is associated with low stomach acid, but ACV may help increase low stomach acid levels and reduce symptoms. Consider shrinking your portion sizes or eating until you’re 80 percent full to prevent the buildup of additional pressure against your lower esophageal valve, suggests Dr. Singh.
5. You Have Food Sensitivities.

If you occasionally feel sick after eating but have some days when you feel okay, you may have a food sensitivity. Common food sensitivities include gluten, dairy, soy, nuts, shellfish, eggs, corn, and FODMAPs, as well as some additives like food dyes and artificial sweeteners.
“When a food sensitivity is present, the immune system reacts to proteins that cause the release of chemicals called mediators—such as histamine, prostaglandins, cytokines—from the white blood cells in the body,” says Yelton. “This mediator release causes inflammation, which can lead to chronic bloating. Unlike allergies, symptoms of food sensitivities can have delayed reactions and can take from 45 minutes to three days to cause symptoms like bloating.”
Try this: First, try to pay specific attention to when your symptoms show up, making note of potential triggers. For example, you might notice that you’re constantly feeling nauseous after eating sugar. If you have a strong suspicion, you can try doing a targeted elimination diet in which you cut out a few potential triggers and then reintroduce them, one by one, after a period of time and note whether that causes an uptick in symptoms, suggests Dr. Singh. Also, consider working with an integrative or functional medicine practitioner who can run food sensitivity testing, says Yelton. These tests aren’t perfect, but they are improving and can help guide you in the right direction and may confirm any food sensitivity suspicions you have.
6. You’re Not Timing Your Meals Correctly.
When you eat matters nearly as much as what you eat—and timing your meals too close together or too far apart can both cause you to feel nauseous after eating. “Eating more frequently doesn’t give your digestive system adequate time to rest, causing sluggishness and bloating,” says Yelton.
That’s because constantly snacking can interfere with something called the migrating motor complex (MMC), which is a cyclic, recurring movement in the stomach and small intestines that aids in the movement of food through the lower GI tract. When your stomach is empty, it recurs every 90-180 minutes, but chronic snacking can inhibit the MMC, slow gastric motility, and potentially contribute to constipation and cramping.
On the other hand, “waiting longer than four hours can cause a dip in blood sugar,” says Yelton. So it’s all about balance.
Try this: “Become a creature of habit and be consistent with when you eat,” says Yelton. “To regulate your blood sugar and support a healthy metabolism, eat regular-sized meals with a balance of protein, fat, and carbs every three to four hours. This allows your digestive system to take a break in between meals and promotes rest and healing for the tissues.”
7. You’re Not Eating Enough Fiber

Not eating enough fiber for a couple of meals, or even a couple of days, probably won’t cause any major problems. But if you’re avoiding roughage on the regular, everything from sluggish digestion to gut dysbiosis can occur—both of which can make you feel pretty bad after you eat.
Fiber, which is present in most whole and minimally-processed plant foods, is key for healthy digestion and bowel habits. “It absorbs water, increases the bulk of your stool, and speeds up movement through the intestine,” says Yelton. “Too little fiber can lead to constipation, which allows toxins to be reabsorbed into your bloodstream, causing inflammation, fatigue, nausea, cramping, and poor gut health.” Additionally, fiber is a food source for the friendly bacteria in your gut. Once these good gut bugs metabolize fiber, they release compounds called short-chain fatty acids (SCFAs), explains Yelton, which have impressive anti-inflammatory and antimicrobial effects that support gut health and overall health.
“Different types of fiber feed different types of bacteria,” says Yelton—so it’s important to get a variety of fibrous foods in your diet such as leafy greens, veggies, fruits, nuts, seeds, and avocados.
Try this: Include at least one fiber-rich food from a different food group with each meal throughout the day. What does this look like? “You might include strawberries in your morning smoothie, add a leafy green vegetable like spinach to your lunch, include whole grains or sweet potatoes with the skin with your dinner, and enjoy a chia seed pudding for dessert,” says Yelton.
8. You have a Thyroid Condition
It might be the last thing you’d suspect, but your thyroid could be what’s making you feel nauseous after eating. Hypothyroidism (or an underactive thyroid) often leads to poor motility, sluggish digestion, and constipation. But post-meal constipation, cramping, and bloating aren’t enough to suggest a thyroid disorder. Because of that, it’s important to pay attention to your other symptoms, too.
“If somebody comes in and says, I have constipation and my skin is really dry, I’m losing more hair than usual, I’m really low energy and fatigued, then the first question I’d ask is, Has anyone checked your TSH (thyroid-stimulating hormone) or thyroid function lately?” says Dr. Singh. “You want to address the underlying hormone problem and then the other symptoms will work themselves out. In the meantime, you can do things to support motility.”
Try this: If you don’t have a diagnosed thyroid disorder but suspect one based on the symptoms, book a doctor’s appointment ASAP. In the meantime, if you’re experiencing sluggish digestion, Dr. Singh recommends regular exercise, post-meal walks, reasonably sized meals, drinking plenty of water, and getting enough fiber in your diet to support digestion and motility.
9. Your Meals Are Too Big
This one might be obvious. Really big meals can make you feel sick—especially if you’re eating them close to bedtime. With the growing popularity of intermittent fasting diets, it’s not unreasonable to think you might go hours and hours without eating only to be a tad overzealous on the portion sizes during your eating window.
But this can cause a buildup of pressure against the lower esophageal valve that separates the esophagus and stomach, allowing stomach acid and food to push back into the esophagus, triggering acid reflux and nausea. And when you do this before bed, you’re not giving your body an opportunity to properly digest. “You’re dumping a large load into your stomach and then shutting down the power plant by sleeping,” says Dr. Singh. “Don’t be surprised if you wake up in the morning and end up burping up your dinner.”
Try this: Eat slowly so your body has time to register how full you really are, or try to stop when you’re about 80 percent full to avoid overeating, and give yourself at least two to three hours between your last meal and bedtime, suggests Dr. Singh. Another idea? Take a digestive enzyme before bigger or heavier meals so your system has extra support. HUM Nutrition’s Flatter Me contains a powerful blend of 18 digestive enzymes to help break down food and prevent bloating.
10. You Have Gallbladder Issues
If you find yourself clutching your stomach and feeling nauseous after eating fried foods or meals high in fat (yes, even the good fats), your gallbladder may be the culprit. “People with gallbladder issues often have an exacerbation of their symptoms when they eat heavier, fattier foods,” says Dr. Singh. “Pain in the right upper abdomen, pain that radiates to the back or shoulder, and nausea and vomiting can occur.”
The gallbladder is a sac that’s located under the liver. It stores and concentrates bile, which aids in the digestion of fat. When you eat foods containing fat, the gallbladder releases bile into the upper part of the small intestines. When someone has gallbladder disease—which often refers to gallstones and cholecystitis (gallbladder inflammation)—these functions are impaired and can cause pain as a result. When gallstones get stuck traveling through the duct that carries bile to the intestines, for example, they block the flow of bile and this can trigger a gallbladder spasm that results in extremely sharp pain.
Interestingly, gallbladder problems are more common in women and experts believe that it’s due to elevated levels of estrogen.
Try this: If symptoms are severe, you may need gallbladder removal surgery, but often, there are things you can do to prevent gallstones and their symptoms. Avoiding foods with excessive amounts of fat, like fried foods, keeping your portion sizes reasonable, and taking a digestive enzyme containing lipase (which breaks down fat) before meals may help, according to Dr. Singh. Research has also shown that women who eat more fiber and have several servings of nuts per week are less likely to need gallbladder surgery.